AstraZeneca study shows SGLT-2 inhibitors significantly reduced hospitalizations for heart failure and death

Landmark real-world evidence from an international study of more than 300,000 patients with type-2 diabetes showed treatment with SGLT-2 inhibitors reduced risk of hospitalization for heart failure by 39% and all-cause mortality by 51%.
AstraZeneca has announced results of the first large real-world evidence study of its kind evaluating the risk of hospitalization for heart failure and death from any cause in patients with type-2 diabetes (T2D) receiving treatment with a newer class of diabetes medicines, SGLT-2 inhibitors (SGLT-2i).
The CVD-REAL study assessed data from more than 300,000 patients across six countries, 87% of whom did not have a history of cardiovascular disease. The data showed that across this broad population of patients with T2D compared to other T2D medicines, treatment with SGLT-2i medicines - Farxiga (dapagliflozin), canagliflozin, empagliflozin - reduced the rate of hospitalization for heart failure by 39% and death from any cause by 51%. For the composite endpoint of hospitalization for heart failure and death from any cause, the reduction was 46%
.Bruce Cooper, Vice President and Head of Global Medical Affairs at AstraZeneca, said: “Diabetes is a growing epidemic worldwide, which is associated with significant comorbidities that contribute to an increased risk of costly hospitalizations and even death. Real-world data from this study provide striking evidence that the newer SGLT-2i class of medicines cuts the rate of hospitalizations for heart failure and death by approximately half. CVD-REAL is the first study to observe these effects of SGLT-2i treatment in a much broader and lower risk group of type-2 diabetes patients than previously evaluated in clinical trials.”
The hospitalizations for heart failure analysis was conducted using anonymized patient data from Denmark, Germany, Norway, Sweden, UK and the US. Of the data reviewed, 41.8% of patients were on Farxiga (dapagliflozin), 52.7% on canagliflozin and 5.5% on empagliflozin. The analysis of death from any cause was conducted using anonymized patient data from Denmark, Norway, Sweden, UK and the US. Of the data reviewed, 51.0% of patients were on Farxiga (dapagliflozin), 42.3% on canagliflozin and 6.7% on empagliflozin.
This is the first of several comparative analyses of CVD-REAL. The study is ongoing and future analyses will be conducted using this dataset as well as data from additional countries. The data for this study were obtained from real-world sources including medical records, claims databases and national registers, and were not independently adjudicated or verified against source documents. The analysis was validated by the independent academic statistical group at St. Luke’s Mid America Heart Institute, Kansas City, US. While CVD-REAL was a large study with a robust propensity-matching technique, given its observational nature the possibility of residual, unmeasured confounding factors cannot be definitively excluded.
Farxiga (dapagliflozin) is indicated as an adjunct to diet and exercise to improve glycemic control in adults with type-2 diabetes. Farxiga is not indicated to reduce the risk of CV events, death or hospitalization for heart failure. There have been no clinical trials establishing conclusive evidence of macrovascular risk reduction with Farxiga. The dapagliflozin cardiovascular outcomes trial, DECLARE, is ongoing and expected to provide data in 2019 at the latest.
Related News
-
News CPHI Frankfurt 2022: Innovator Interview – DSM Biomedical
At CPHI Frankfurt we spoke to Anne-Cecile Bayne, Global Science & Innovation Lead Pharma and Medical Nutrition, and Marc Hendriks, Vice President Strategy & Business Development, on their expertise in nitrosamines and business strategy at DSM Biomedica... -
News New WHO health emergency guidelines expect full transparency from Big Pharma
The WHO are proposing a new set of pandemic guidelines to set out how future global health crises should be handled. -
News Magic mushrooms could be used to treat mental health conditions
A compound found in magic mushrooms, psilocybin, could be used to treat mental health conditions and help patients suffering with severe depression, as shown by the results of the largest study of its kind to date. -
News UK-based partnership to launch DETERMINE study into rare cancer research
UK-based CRO Quanticate is set to partner with Cancer Research UK for the launch of the DETERMINE study focused on testing a range of existing and approved drugs and therapies on rare cancers. -
News FDA approves Thermo Fisher blood tests for wheat and sesame allergies
Both tests have been approved by the US regulator for in vitro diagnostic use -
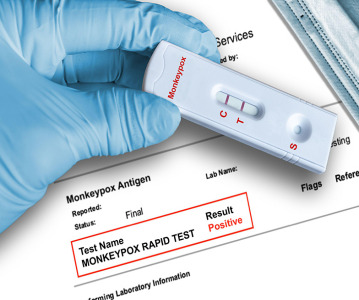
News QIAGEN launches world’s first syndromic test for monkeypox
The test can distinguish between monkeypox and other diseases that cause similar symptoms. -
News Monkeypox Update: Vaccine shortage, sewage surveillance and global testing
As concern over the monkeypox outbreak continues to rise, we take a look at major developments from the first week of August. -
News CPHI Podcast Series: The importance of novel excipients for innovative drug development
The latest episode in the CPHI Podcast Series dives into the world of novel excipients and explores their importance for innovative drug development.
Position your company at the heart of the global Pharma industry with a CPHI Online membership
-
Your products and solutions visible to thousands of visitors within the largest Pharma marketplace
-
Generate high-quality, engaged leads for your business, all year round
-
Promote your business as the industry’s thought-leader by hosting your reports, brochures and videos within your profile
-
Your company’s profile boosted at all participating CPHI events
-
An easy-to-use platform with a detailed dashboard showing your leads and performance


.png)