Possible new treatment for Ewing sarcoma
Discovery of a new drug with high potential to treat Ewing sarcoma, an often deadly cancer of children and young adults.
Discovery of a new drug with high potential to treat Ewing sarcoma, an often deadly cancer of children and young adults, and the previously unknown mechanism behind it, come hand-in-hand in a new study by researchers from Huntsman Cancer Institute (HCI) at the University of Utah. The report appears in the online issue of the journal Oncogene.
"Ewing sarcoma is almost always caused by a cancer-causing protein called EWS/FLI," said Stephen Lessnick, M.D., Ph.D., director of HCI's Center for Children's Cancer Research, professor in the Department of Pediatrics at the University of Utah School of Medicine, and an HCI investigator.
In the lab, Lessnick and his colleagues found that an enzyme, called lysine specific demethylase (LSD-1), interacts with EWS/FLI to turn off gene expression in Ewing sarcoma. By turning off specific genes, the EWS/FLI-LSD1 complex causes Ewing sarcoma development. "This makes LSD-1 an important target for the development of new drugs to treat Ewing sarcoma," Lessnick said.
"For a long time, we've known that EWS/FLI works by binding to DNA and turning on genes that activate cancer formation," said Lessnick. "It was a surprise to find out that it turns genes off as well.
"The beauty, if there's anything beautiful about a nasty disease like this, is that if we can inhibit EWS/FLI, we can inhibit this cancer, because EWS/FLI is the master regulator of Ewing sarcoma," Lessnick added.
While Lessnick and his colleagues worked on EWS/FLI in their basic science lab, Sunil Sharma, M.D., director of HCI's Center for Investigational Therapeutics, professor in the Department of Medicine at the University of Utah, and an HCI investigator, had already focused on LSD-1 as a possible target for new cancer treatments and had been working for several years to design drugs that would inhibit its actions.
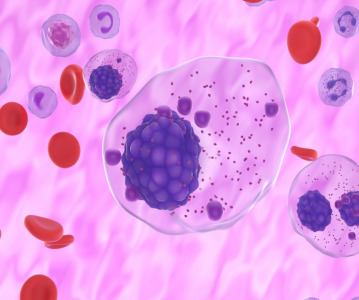
"We had found that LSD-1 was important for regulation of a variety of properties in several different cancers, including acute leukemias, breast and prostate cancers," Sharma said.
"After Steve showed that LSD-1 was directly regulating the function of EWS/FLI, we teamed up with him to see whether the LSD inhibitors we had discovered worked in Ewing sarcoma models," Sharma said. "Our tests in Ewing sarcoma tissue cultures show they are extremely potent."
Lessnick and Sharma are now working together to further test LSD inhibitors in animal models as they work toward approval of a first-in-man clinical trial. In addition, Lessnick's basic science research on LSD-1 in Ewing sarcoma continues. "We think it may play a larger role in Ewing sarcoma than simply turning off a handful of genes, and we're looking into that," said Lessnick.
"This is a great example of how collaboration between the therapeutics and basic science programs can lead to new treatments for patients—one of HCI's highest goals," said Sharma.
Graduate student Savita Sankar of the Lessnick lab was instrumental in this research; her work is supported by the Howard Hughes Medical Institute (HHMI) under the University of Utah Med into Grad Program. This work was also supported by NIH/NCI grants R01 CA140394 and P30 CA042014, as well as funding from the Imaging, Diagnostics, and Therapeutics Program at Huntsman Cancer Institute. Work in the Lessnick lab is also supported by Sydney's Incredible Defeat of Ewing's Sarcoma (SIDES).
The mission of Huntsman Cancer Institute (HCI) at the University of Utah is to understand cancer from its beginnings, to use that knowledge in the creation and improvement of cancer treatments, to relieve the suffering of cancer patients, and to provide education about cancer risk, prevention, and care. HCI is a National Cancer Institute-Designated Cancer Center, which means that it meets the highest national standards for cancer care and research and receives support for its scientific endeavors. HCI is also a member of the National Comprehensive Cancer Network (NCCN), a not-for-profit alliance of the world's leading cancer centers that is dedicated to improving the quality and effectiveness of care provided to patients with cancer.
Related News
-
News BioNTech to begin mRNA vaccine manufacturing in Rwanda by 2025
German biotechnology company BioNTech has stated their intentions to begin production at their mRNA vaccine factory in Rwanda by 2025, which will mark the first foreign mRNA vaccine manufacturing site on the continent of Africa. -
News Identifying Alzheimer’s Disease biomarker proteins with whole blood tests
A University of Manchester spin-out pharmaceutical company, PharmaKure, has reported successful study results for the quantification of Alzheimer’s Disease biomarker proteins with a whole blood test. -
News Bill & Melinda Gates Foundation to boost mRNA vaccine initiatives in Africa with USD $40m
To address vaccine inequality and accessibility issues, the Bill & Melinda Gates Foundation aims to deliver USD $40m to various biotech companies and vaccine manufacturers in support of mRNA vaccine development. -
News CPHI Podcast Series: Exploring neurological frontiers in Alzheimer's and beyond
The next episode of the CPHI Podcast Series delves into the science and background behind some recent developments in the field of Alzheimer's disease and neurological disorders. -
News Is patient centricity the future of pharmaceutical manufacturing?
In this interview with Sandra Sánchez y Oldenhage, President of PharmAdvice, she speaks to the importance of considering patients in the manufacturing stages of the pharmaceutical supply chain, and how it can redefine healthcare. -
News CPHI Podcast Series: How to leverage AI for Drug Discovery
Artificial intelligence is the topic of debate in the latest episode from the CPHI Podcast Series, where Digital Editor Lucy Chard speaks with Bill Whitford of DPS Group about the integration of AI in healthcare. -
News Pfizer forges ahead with blood cancer therapy after approval from FDA
Pfizer gains accelerated approval from the US FDA for their new bispecific antibody therapy for multiple myeloma, set to address an unmet need for patients. -
News Alzheimer's drug donanemab deemed effective in landmark clinical trial
Results from the TRAILBLAZER-ALZ 2 Randomised Clinical Trial into the use of donanemab to treat early symptoms of Alzheimer’s disease have been analysed.
Position your company at the heart of the global Pharma industry with a CPHI Online membership
-
Your products and solutions visible to thousands of visitors within the largest Pharma marketplace
-
Generate high-quality, engaged leads for your business, all year round
-
Promote your business as the industry’s thought-leader by hosting your reports, brochures and videos within your profile
-
Your company’s profile boosted at all participating CPHI events
-
An easy-to-use platform with a detailed dashboard showing your leads and performance