Magic mushrooms could be used to treat mental health conditions
.png)
A compound found in magic mushrooms, psilocybin, could be used to treat mental health conditions and help patients suffering with severe depression, as shown by the results of the largest study of its kind to date.
In the latest results from a study from COMPASS Pathways, the main ingredient in ‘magic’ mushrooms has been found to reduce symptoms of depression.
This clinical trial was the largest to date to look at the compound, involving 233 patients diagnosed with ‘treatment-resistant’ depression. Treatment-resistant depression is defined as when the patient has not benefitted from the application of at least two antidepressants.
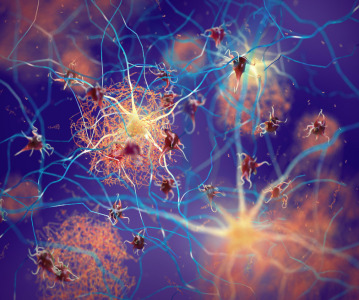
The compound in question is psilocybin, a psychoactive ingredient found in over 200 species of fungi.
The patients involved in the Phase II double-blind trial each received psychological support and then either a 25 mg or 10 mg dose of psilocybin at random, and those in the control group a 1 mg dose.
Psilocybin is thought to affect the areas of the brain that are involved in processing emotions.
When the compound was administered to patients, under controlled conditions, it was reported that they entered a dream-like state, lasting between 4 and 6 hours.
The results, published in The New England Journal of Medicine, show that those who received the higher dose of psilocybin, 25 mg, demonstrated a significant decrease in depressive symptoms after 3 weeks of treatment (the primary end point), compared to those in the lower dose treatment groups. In this 25 mg dose group, the incidence of remission in patients was 29%, compared to 9% and 8% in the 10 mg and 1 mg groups respectively.
However, between weeks 3 and 12 of treatment (with 12 weeks being the secondary end point), the difference in response between the groups was not statistically significant. Overall in the 25 mg study group 16% of patients showed a sustained response, i.e a response that was held from week 3 through to week 12.
The trial's findings are positive but not ground-breaking, advised Ravi Das, associate professor at the University College London Institute of Mental Health, UK.
"There were an uneven number of severely depressed patients in each group; with significantly fewer severely depressed people in the apparent 'effective' (25mg) dose group. This does not appear to be acknowledged in the paper."
The trial wasn’t without concerns, several of the patients experienced adverse side effects; in the 25 mg group patients reported headaches (24%), nausea and dizziness and fatigue. In a smaller proportion, severe adverse effects were reported, including suicidal ideation, intentional self-harm behaviour and hospitalisation due to severe depression.
By studying depression, suicidality is going to be a feature of the illness course, stated Guy Goodwin, chief medical officer at COMPASS Pathways (London, UK).
"Our hypothesis is that the differences are by chance...but we can only settle this by doing further experiments."
Goodwin also mentioned that the compound was being tested in two other late-stage trials looking at its effectiveness as a treatment for PTSD and anorexia nervosa, with hopes the results could be released at the end of 2024.
The use of these drugs for treatment of mental health conditions remains controversial, but the latest research shows that it worth investigating further.
Related News
-
News Pharmapack Awards 2024 Patient-Centric Design Award Winner – Dr Ferrer BioPharma
The 2024 Pharmapack Awards celebrated the best in innovation and design for the pharmaceutical packaging and drug delivery industry on January 24, 2024. -
News Pharmapack 2024 - From the Floor
Paris once again welcomes Europe’s leading trade show in pharmaceutical packaging and drug delivery innovation. Join our content team as Pharmapack 2024 opens its doors to leading experts and innovators in pharmaceutical packaging and drug delive... -
News On Track at Pharmapack 2024 - The Track Sponsor interview: BD Pharmaceuticals
January 2024 brings both a new year and Europe’s leading packaging and drug delivery event. Bringing the world’s experts in pharmaceutical packaging together in Paris, France, Pharmapack 2024 brings exciting opportunities to learn and colla... -
News CPHI Pharma Awards 2023 – API Development and Innovation Winners: Snapdragon Chemistry, a Cambrex Company
After another year of impressive nominations for the CPHI Pharma Awards our winners were announced at CPHI Barcelona in October. In this series of interviews, we speak to the teams behind the award-winning projects, concepts, and technologies. -
News PharmaKure gains authorisation for next stage testing on Alzheimer's treatment
Clinical stage pharmaceutical company PharmaKure gains permission from UK authorities to enter into further testing for PK051 for the treatment of patients with mild cognitive impairment associated with Alzheimer's disease. -
News New Novo Nordisk AI hub for drug discovery to open in London, UK
Danish pharmaceutical giant Novo Nordisk will be opening an AI-based research facility in the heart of London to advance drug discovery operations. -
News Navigating the Future: Challenges and Opportunities in Pharma Innovation and Investment – CPHI Barcelona 2023 Roundtable Report
In this comprehensive downloadable report, hear from a range of experts in finance and investment in the pharma industry on what investment trends will be shaping the future of the industry, in Catalonia, and the wider world. -
News BioNTech to begin mRNA vaccine manufacturing in Rwanda by 2025
German biotechnology company BioNTech has stated their intentions to begin production at their mRNA vaccine factory in Rwanda by 2025, which will mark the first foreign mRNA vaccine manufacturing site on the continent of Africa.
Position your company at the heart of the global Pharma industry with a CPHI Online membership
-
Your products and solutions visible to thousands of visitors within the largest Pharma marketplace
-
Generate high-quality, engaged leads for your business, all year round
-
Promote your business as the industry’s thought-leader by hosting your reports, brochures and videos within your profile
-
Your company’s profile boosted at all participating CPHI events
-
An easy-to-use platform with a detailed dashboard showing your leads and performance


.png)