NCI study identifies essential genes for cancer immunotherapy

This knowledge could speed the development of a new category of drugs.
A new study identifies genes that are necessary in cancer cells for immunotherapy to work, addressing the problem of why some tumours don’t respond to immunotherapy or respond initially but then stop as tumour cells develop resistance to immunotherapy.
The study, from the National Cancer Institute (NCI [part of the National Institutes of Health]), was led by Nicholas Restifo, a senior investigator with NCI’s Center for Cancer Research, with coauthors from NCI; Georgetown University, Washington DC; the Broad Institute of MIT and Harvard University, Cambridge, Massachusetts; New York University, New York City; and the University of Pennsylvania, Philadelphia. It was published online in Nature on 7 August 2017.
“There is a great deal of interest in cancer immunotherapy, especially for patients who have metastatic cancer,” said Dr Restifo. “The response to immunotherapy can be fantastic, but understanding why some patients don’t respond will help us improve treatments for more patients.”
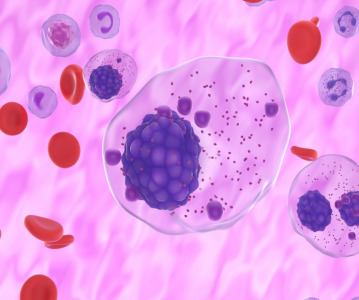
Cancer immunotherapy relies on T cells, a type of cell in the immune system, to destroy tumours. Dr Restifo and his colleagues have previously shown that the infusion of large numbers of T cells can trigger complete regression of cancer in patients. They and others have also shown that T cells can directly recognize and kill tumour cells.
However, some tumour cells are resistant to the destruction unleashed by T cells. To investigate the basis for this resistance, the researchers sought to identify the genes in cancer cells that are necessary for them to be killed by T cells.
Working with a melanoma tumour cell line, the researchers used a gene editing technology called CRISPR that “knocks out,” or stops the expression, of individual genes in cancer cells. By knocking out every known protein-encoding gene in the human genome and then testing the ability of the gene-modified melanoma cells to respond to T cells, they found more than 100 genes that may play a role in facilitating tumour destruction by T cells.
Once the team identified these “candidate” genes, they sought additional evidence that these genes play a role in susceptibility to T cell-mediated killing. To this end, they examined data on “cytolytic activity,” or a genetic profile that shows cancer cells are responding to T cells, in more than 11,000 patient tumours from The Cancer Genome Atlas, a collaboration between NCI and the National Human Genome Research Institute, also part of NIH. They found that a number of the genes identified in the CRISPR screen as being necessary for tumour cells to respond to T cells were indeed associated with tumour cytolytic activity in patient samples.
One such gene is called APLNR. The product of this gene is a protein called the apelin receptor. Although it had been suspected to contribute to the development of some cancers, this was the first indication of a role in the response to T cells. Further investigation of tumours from patients resistant to immunotherapies showed that the apelin receptor protein was nonfunctional in some of them, indicating that the loss of this protein may limit the response to immunotherapy treatment.
Shashank Patel, the first author of the study, said the results show that “many more genes than we originally expected play a vital role in dictating the success of cancer immunotherapies.”
The researchers wrote that this gene list could serve as a blueprint to study the emergence of tumour resistance to T cell-based cancer therapies. Dr Restifo noted that if this set of genes is validated in clinical trials, then this data could eventually lead to more effective treatments for patients.
NI“If we can truly understand mechanisms of resistance to immunotherapy, we might be able to develop new therapeutics,” he said. “In fact, in the future, this knowledge could speed the development of a new category of drugs that can circumvent these escape mechanisms of tumour cells and help patients experience complete responses.”
Related News
-
News BioNTech to begin mRNA vaccine manufacturing in Rwanda by 2025
German biotechnology company BioNTech has stated their intentions to begin production at their mRNA vaccine factory in Rwanda by 2025, which will mark the first foreign mRNA vaccine manufacturing site on the continent of Africa. -
News Identifying Alzheimer’s Disease biomarker proteins with whole blood tests
A University of Manchester spin-out pharmaceutical company, PharmaKure, has reported successful study results for the quantification of Alzheimer’s Disease biomarker proteins with a whole blood test. -
News Bill & Melinda Gates Foundation to boost mRNA vaccine initiatives in Africa with USD $40m
To address vaccine inequality and accessibility issues, the Bill & Melinda Gates Foundation aims to deliver USD $40m to various biotech companies and vaccine manufacturers in support of mRNA vaccine development. -
News CPHI Podcast Series: Exploring neurological frontiers in Alzheimer's and beyond
The next episode of the CPHI Podcast Series delves into the science and background behind some recent developments in the field of Alzheimer's disease and neurological disorders. -
News Is patient centricity the future of pharmaceutical manufacturing?
In this interview with Sandra Sánchez y Oldenhage, President of PharmAdvice, she speaks to the importance of considering patients in the manufacturing stages of the pharmaceutical supply chain, and how it can redefine healthcare. -
News CPHI Podcast Series: How to leverage AI for Drug Discovery
Artificial intelligence is the topic of debate in the latest episode from the CPHI Podcast Series, where Digital Editor Lucy Chard speaks with Bill Whitford of DPS Group about the integration of AI in healthcare. -
News Pfizer forges ahead with blood cancer therapy after approval from FDA
Pfizer gains accelerated approval from the US FDA for their new bispecific antibody therapy for multiple myeloma, set to address an unmet need for patients. -
News Alzheimer's drug donanemab deemed effective in landmark clinical trial
Results from the TRAILBLAZER-ALZ 2 Randomised Clinical Trial into the use of donanemab to treat early symptoms of Alzheimer’s disease have been analysed.
Position your company at the heart of the global Pharma industry with a CPHI Online membership
-
Your products and solutions visible to thousands of visitors within the largest Pharma marketplace
-
Generate high-quality, engaged leads for your business, all year round
-
Promote your business as the industry’s thought-leader by hosting your reports, brochures and videos within your profile
-
Your company’s profile boosted at all participating CPHI events
-
An easy-to-use platform with a detailed dashboard showing your leads and performance