Nitrosamine contamination: pharma’s re-evaluation of its supply chain

The detection of nitrosamine impurities in some finished dosages has opened up a whole new set of challenges for API manufacturers who need to perform risk evaluations of their processes
While the pharmaceutical industry is no stranger to regulatory compliance, it could be argued that the lion’s share of the scrutiny up till now has fallen mainly on the ‘bookends’ of the product lifecycle: research and development and in the commercialization stage just before launch.
However, the recent detection of nitrosamine contamination in pharmaceutical finished dosages has opened up the pharmaceutical supply chain to a different set of challenges and problems altogether. Up until now, the chemistry assessment of any product has occurred during development and just before launch with less happening on the active pharmaceutical ingredients (API) processing side during the manufacturing process.
That has now all changed. API manufacturers are now finding themselves needing to stay on top of what has developed into a continuous regulatory process which is having a profound impact on their raw materials sourcing and processing conditions.
The NDMA cancer risk
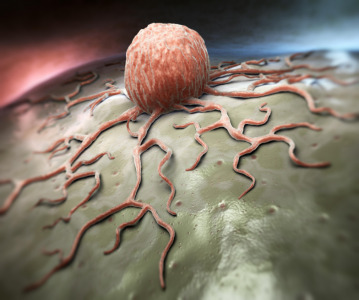
Nitrosamines are genotoxic substances which may increase the risk of cancer in people exposed to above acceptable levels over longer periods of time. One of these, N-Nitrosodimethylamine (NDMA), a chemical form of nitrosamine, is classified as a potential human carcinogen and a likely cause of cancer. The US Food and Drug Administration (FDA) first detected it in angiotensin II receptor blockers (ARBs) – used to treat high blood pressure and heart illness and commonly known as the sartans – back in 2018.
In the summer of 2019, the FDA became aware of independent laboratory testing that found low levels of NDMA in heartburn drug ranitidine (brand name Zantac). It swiftly issued a warning to the public of the potential risks and to consider alternative OTC and prescription treatments while at the same time requesting ranitidine formulation manufacturers withdraw all prescription and OTC versions from the market immediately.
At the time, the agency said while it had not observed unacceptable levels of NDMA in many of the samples it tested, it issued the caveat that “since we don't know how or for how long the product might have been stored, we decided that it should not be available to consumers and patients unless its quality can be assured.”
Since then, a chain reaction of voluntary product recalls has been set in motion, the very latest in April 2020 from Amneal Pharmaceuticals, which recently pulled three lots of ulcer and heartburn treatment, nizatidine, from the shelves.
Amneal’s response was typical of those that came before it from other affected drug producers; couching it as a precautionary measure, the company stressed that it had not received any reports of adverse events that had been confirmed to be directly related to the recall.
Also in April, the FDA ordered manufacturers to withdraw all prescription and over-the-counter versions of ranitidine from the market immediately. The US regulator is now conducting ongoing investigations into the presence of nitrosamine in other drug products including metformin, an oral drug used to control high blood sugar in patients with type II diabetes. However, in this case, there have been no recalls of metformin yet, with the FDA saying levels founds in other countries so far are in the range naturally occurring in some foods including cured and grilled meats, dairy products and pickled vegetables and water.
EMA review
A European Medicines Agency (EMA) Article 31 review of sartans at risk of containing nitrosamine impurities concluded that manufacturers must review and make necessary changes to their manufacturing processes to minimize their presence as much as possible. In addition, strict limits were set for nitrosamines in these products.
The findings of the review indicated that there is a potential for nitrosamines to be present in APIs for other medicines, depending on the API and the finished product manufacturing processes.
The EMA has issued new guidelines requesting market authorization holders to not only conduct testing of all at-risk medicines for nitrosamines, but also to complete risk evaluations identifying potentially affected products, which essentially means going through their API manufacturing and ingredients sourcing with a fine-tooth comb. The deadline for the latter request was initially 26 March 2020 but has since been extended to 1 October 2020 presumably due to the current COVID-19 pandemic.
Huge sea-change
Pharmaceutical company, Dr. Reddy’s Laboratories, was one of the very first API manufacturers to instigate a complete review to ensure that nitrosamine impurities are avoided by design and analytical methods are in place which meet the future stringent limits which have been set by regulatory agencies.
On winning the API Supplier of the Year award at Generics Bulletin’s Annual Global Generics & Biosimilars Awards hosted during CPHI Worldwide in Frankfurt last November, the company was commended for its proactive and methodical approach in addressing the global sartan APIs concern.
The swathe of enforcements and investigative scrutiny by regulators has been a huge sea-change for API manufacturers, who not only have to examine their own processes but must also ensure that the key starting materials they source have a clean bill of health, as Rajesh Sadanandan, Region Head – North America & Europe API, Dr Reddy’s, explains.
“This presents a different set of challenges and problems to the pharmaceutical supply chain,” he says. “These new reviews will be a continuous process and will have a massive impact on raw material sourcing and processing conditions.”
He adds that tighter controls of key starting materials will further add to the complexity and the volume of key data required by API manufacturers from starting material vendors: “2020 will show how companies are prepared to keep up with these new regulations and challenges. It’s a collaborative effort of starting material, API and finished formulation manufacturers.”
One such company that is reacting to the new regulatory environment is India’s SMS Pharma, a large manufacturer of generic ranitidine. The firm says it has completed a detailed risk assessment study for the formation of NDMA impurity in its ranitidine hydrochloride drug substance and has found that the impurity level increases the longer the drug is in storage.
“Based on the risk assessment study, we have modified the process of Ranitidine HCl drug substance to control the NDMA impurity during the storage and the modified process details have been submitted to the FDA,” an SMS Pharma spokesman says, describing the modified process material as more stable and the NDMA impurity “well controlled.”
Effective testing
The urgent call to action effectively means pharma manufacturers are having to rigorously examine all stages of their processes to ensure there are no ‘ways in’ for nitrosamine impurities to their medicines.
Andrew James, marketing director at Ellutia, a company that produces what it describes as the ‘industry standard’ for nitrosamine detection, the 800 Series TEA, says that since the final quarter of 2019, the firm has been inundated with requests from Big Pharma companies keen to understand what testing technologies are out there.
He describes the 800 Series TEA as a detector that can be interfaced to a gas chromatograph to attain speciated analysis results identifying each individual nitrosamine present and the quantity that’s there.
“Where we’ve seen a lot of pharma interest for the TEA is its ability to rapidly test for apparent total nitrosamine content (ATNC) rather than separating nitrosamines, “ he says.
He goes on to explain that a total value below the regulatory threshold means the tested sample can be deemed safe, while if the ATNC tests above the level, it can be then moved on for further analysis to find out which nitrosamines are present and in what quantities.
Identifying the numerous potential risk-points throughout the manufacturing process of pharmaceutical drugs whereby nitrosamines could enter into the product is likely to be the biggest challenge for API manufacturers going forward.
“Generally, nitrosamines are formed wherever there are secondary amines present and a nitrate ion - these can be formed during some of the manufacturing processes depending on what solvents are being used in the manufacture of APIs,” says James, adding that nitrosamines may be introduced directly from sources that companies may not yet have considered such as water and packaging.
So will the evolving set of requirements around nitrosamine impurities prove too burdensome for pharma companies and API manufacturers as they seek to navigate to calmer waters?
Rajesh Sadanandan at Dr Reddy’s doesn’t think so: “It might be tough, but also provides a competitive edge for those manufacturers who already proactively have assessed their processes including starting material manufacturing. Pharma companies, API suppliers and ingredients manufacturer with a strong patient-focused culture are typically best positioned to anticipate and respond to these challenges, which ultimately will increase both access to high quality medications as well as patient health.”
Related News
-
News mRNA therapy for ovarian cancer and muscle wasting
Researchers demonstrate results of a promising mRNA therapy for ovarian cancer and muscle wasting caused by cachexia, a condition associated with various types of cancers and chronic diseases. -
News Pfizer CentreOne Content Refinement Q3 media buy
For 40 years Pfizer CentreOne has been guiding drug projects to success. Here’s how our services make us an altogether different kind of CDMO: -
News Bora Pharmaceuticals expands development and manufacturing capacity with landmark acquisition
Taiwan-based CDMO Bora Pharmaceuticals have acquired niche generic drugs developer TWi Pharmaceuticals, expanding their outsourced development and manufacturing services with two additional manufacturing facilities. -
News Lonza and Touchlight collaboration to bring expanded end-to-end mRNA offerings
Through a collaboration with biotech company Touchlight, Lonza is set to expand their end-to-end offering for mRNA manufacturing with additional DNA raw material sources, including Touchlight’s doggybone DNA. -
News Oxford University presents promising phase II data for malaria vaccine
The malaria vaccine R21/Matrix-M, developed by researchers at Oxford University, has produced encouraging new data for the global effort against the mosquito-borne disease. -
News NextPharma to acquire Norway manufacturing site from Takeda
Biopharmaceutical company Takeda and CDMO NextPharma have announced an acquisition agreement in which Takeda will divest from their Asker, Norway manufacturing site, set to be acquired by NextPharma. -
News Gut instinct: molecular link between COVID-19 and serotonin cells in the gut
New research may provide further evidence of the gut’s role in SARS-CoV-2 infection and disease severity with a molecular link between serotonin-producing cells in the gut and COVID-19 disease severity. -
News Novavax COVID-19 vaccine receives backing from European Medicines Agency
The European Medicines Agency has backed the Nuvaxovid COVID-19 vaccine for adults as a booster shot to other COVID-19 vaccines.
Position your company at the heart of the global Pharma industry with a CPHI Online membership
-
Your products and solutions visible to thousands of visitors within the largest Pharma marketplace
-
Generate high-quality, engaged leads for your business, all year round
-
Promote your business as the industry’s thought-leader by hosting your reports, brochures and videos within your profile
-
Your company’s profile boosted at all participating CPHI events
-
An easy-to-use platform with a detailed dashboard showing your leads and performance

.png)
.png)
.png)

.png)
.png)