Researchers develop less toxic anti-cancer drug
The novel drug enters the ‘powerhouses’ of cancer cells to launch an attack, without harming healthy cells.
New drug works like a ‘magic bullet’ that is delivered directly to the mitochondria of cancer cells.
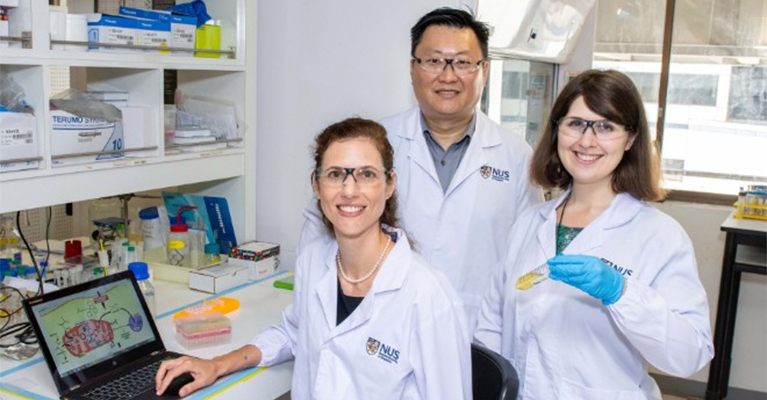
A team of National University of Singapore (NUS) pharmacists and chemists has developed a new anti-cancer drug that has less toxic effects to the kidneys.
The new drug works like a ‘magic bullet’ that is delivered directly to the mitochondria — the power generators of cells — of cancer cells. Once the drug reaches the tumour, two active molecules — an anti-cancer drug and a sensitizer — are released at once, and they attack the mitochondria, leading to the death of cancer cells. Such a targeted approach reduces the drug’s interactions with other tissues, minimising side effects and it is expected to lower the risk of patients developing resistance to anti-cancer drugs like cisplatin.
“When designing and evaluating new cancer treatments, researchers often use cisplatin as a gold standard to compare new medicines. Cisplatin is known to kill cancer cells by damaging DNA. But cancer cells are smart, and they have ways to repair this damage and become resistant to the drug treatment. Hence, we need good alternatives that can address drug resistance and the associated side effects,” explained Associate Professor Ang Wee Han from NUS Chemistry.
He worked together with Associate Professor Giorgia Pastorin from NUS Pharmacy to look into developing an anti-cancer drug with better treatment outcomes to serve as an alternative to cisplatin. The research was conducted in collaboration with Professor Dan Gibson from The Hebrew University of Jerusalem.
Tumour disappears after targeted delivery of new drug
Recognising that the mitochondria have less efficient repair mechanisms in their DNA, the NUS team came up with a novel drug that can be delivered directly to them. This was achieved by adding a mitochondria-targeting ligand to the original cisplatin scaffold. This additional ligand has a strong positive charge that displays high affinity towards the complementary negative charge of the mitochondrial membrane.
The NUS researchers examined how their drug was released into the blood, and came up with a method to encapsulate their novel drug formulation in miniaturised drug carriers known as liposomal nanovesicles. As tumours grow very rapidly, their blood vessels do not have time to develop properly and they are leaky. Such an environment enables the permeation of the drug carriers from blood vessels to the tumour microenvironment, and be retained within the tumour to carry out the ‘attack’ on cancer cells.
Experiments by the researchers showed that the new drug, when delivered in a colon cancer model, shrank the tumour until it became impalpable.
“No sign of kidney inflammation was detected, unlike the use of conventional cisplatin. These results indicate that our invention is a viable alternative to cisplatin,” said Dr Maria Babak, who was the first author of the study.
“While our results show great potential, we want to further challenge ourselves to improve our drug so that we can achieve complete tumour remission and tackle drug resistance. Accomplishing such a feat will open doors to improving cancer treatment and survival rates,” said Assoc Prof Pastorin.
To improve the efficacy of the new drug, the research team is looking into adjusting the doses and frequencies of the treatment. They are also studying combinations of different anti-cancer drugs, and examining ways to packaging them into suitable drug delivery systems to increase efficacy, decrease side effects and tackle drug resistance among cancer patients.
Related News
-
News Eli Lilly gets ready to launch five new drugs in 2023
Eli Lilly, the American pharmaceutical company (IN, USA) are gearing up for a big year ahead, with hopes to launch five new drugs and capitalise on growing obesity and Alzheimer’s disease markets. -
News Amgen buys Horizon for $27.8 billion in bold step into the rare disease market
Amgen Inc buys pharmaceutical company Horizon Therapeutics in a multibillion-dollar deal, in hopes to capitalise on it's portfolio of drugs in the highly sort after rare disease market. -
News Pharma Supply Chain People Moves
The latest appointments and promotions across the pharmaceutical supply chain. -
News Merck to donate new Ebola vaccine to defend against outbreaks in Uganda
Pharmaceutical giant Merck has announced they will be speeding up the processing of a new vaccine against the latest strain of the Ebola virus, to be donated to a global non-profit organisation for distribution -
News CPHI Podcast Series: Driving innovation with pharmaceutical startups
The latest episode in the CPHI Podcast Series explores how startups are driving innovation by taking high-risk approaches and doing business with greater agility. -
News Greener and efficient processes: Quaternary Ammonium Salts
Quaternary Ammonium Salts play a crucial part in Organic Chemistry processes at many major industries. Discover why.
-
News Biosimilars save patients $11B annually, but barriers to adoption remain in US market
Biosimilars introduce competition into the biologics market, driving down prices and increasing patient access. -
News WHO recommends use of two monoclonal antibody treatments against Ebola
The health body recommended use of treatments by Regeneron and Ridgeback Bio
Position your company at the heart of the global Pharma industry with a CPHI Online membership
-
Your products and solutions visible to thousands of visitors within the largest Pharma marketplace
-
Generate high-quality, engaged leads for your business, all year round
-
Promote your business as the industry’s thought-leader by hosting your reports, brochures and videos within your profile
-
Your company’s profile boosted at all participating CPHI events
-
An easy-to-use platform with a detailed dashboard showing your leads and performance



.png)