NIH launches first US clinical trial of patient-derived stem cell therapy to replace dying cells in retina

NEI-led study to test safety of treatment for a form of age-related macular degeneration that currently lacks treatment.
Researchers at the National Eye Institute (NEI) are launching a clinical trial to test the safety of a novel patient-specific stem cell-based therapy to treat geographic atrophy, the advanced “dry” form of age-related macular degeneration (AMD), a leading cause of vision loss among people age 65 and older. The geographic atrophy form of AMD currently has no treatment.
“The protocol, which prevented blindness in animal models, is the first clinical trial in the US to use replacement tissues from patient-derived induced pluripotent stem cells (iPSC),” said Kapil Bharti, a senior investigator and head of the NEI Ocular and Stem Cell Translational Research Section. The NEI is part of the National Institutes of Health.
The therapy involves taking a patient’s blood cells and, in a lab, converting them into iPS cells, which have the potential to form any type of cell in the body. The iPS cells are programmed to become retinal pigment epithelial (RPE) cells, the type of cell that dies early in the geographic atrophy stage of macular degeneration. RPE cells nurture photoreceptors, the light-sensing cells in the retina. In geographic atrophy, once RPE cells die, photoreceptors eventually also die, resulting in blindness. The therapy is an attempt to shore up the health of remaining photoreceptors by replacing dying RPE with iPSC-derived RPE.
Before they are transplanted, the iPSC-derived RPE are grown in sheets one cell thick, replicating their natural structure within the eye. This monolayer of iPSC-derived RPE is grown on a biodegradable scaffold designed to promote the integration of the cells within the retina. Surgeons position the patch between the RPE and the photoreceptors using a surgical tool designed specifically for that purpose.
Under the Phase I/IIa clinical trial protocol 12 patients with advanced-stage geographic atrophy will receive the iPSC-derived RPE implant in one of their eyes and be closely monitored for a period of at least one year to confirm safety.
A concern with any stem cell-based therapy is its oncogenic potential: the ability for cells to multiply uncontrollably and form tumours. In animal models, the researchers genetically analysed the iPSC-derived RPE cells and found no mutations linked to potential tumour growth.
Furthermore, the use of an individual’s autologous (own) blood cells is expected to minimize the risk of the body rejecting the implant.
Should early safety be confirmed, later study phases will include more patients to assess the efficacy of the implant to prevent blindness and restore vision in patients with geographic atrophy.
An FDA requirement for moving forward with the clinical trial was the establishment of GMP protocols to ensure that the iPSC-derived RPE are a clinical-grade product. GMP protocols are key for making the therapy reproducible and for scaling up production should the therapy receive FDA approval.
The preclinical research for the trial was supported by the NEI Intramural Research Program and by an NIH Common Fund Therapeutic Challenge Award. The trial is being conducted at the NIH Clinical Center in Bethesda, MD.
Related News
-
News CPHI Frankfurt 2022: Innovator Interview – DSM Biomedical
At CPHI Frankfurt we spoke to Anne-Cecile Bayne, Global Science & Innovation Lead Pharma and Medical Nutrition, and Marc Hendriks, Vice President Strategy & Business Development, on their expertise in nitrosamines and business strategy at DSM Biomedica... -
News New WHO health emergency guidelines expect full transparency from Big Pharma
The WHO are proposing a new set of pandemic guidelines to set out how future global health crises should be handled. -
News Magic mushrooms could be used to treat mental health conditions
A compound found in magic mushrooms, psilocybin, could be used to treat mental health conditions and help patients suffering with severe depression, as shown by the results of the largest study of its kind to date. -
News UK-based partnership to launch DETERMINE study into rare cancer research
UK-based CRO Quanticate is set to partner with Cancer Research UK for the launch of the DETERMINE study focused on testing a range of existing and approved drugs and therapies on rare cancers. -
News FDA approves Thermo Fisher blood tests for wheat and sesame allergies
Both tests have been approved by the US regulator for in vitro diagnostic use -
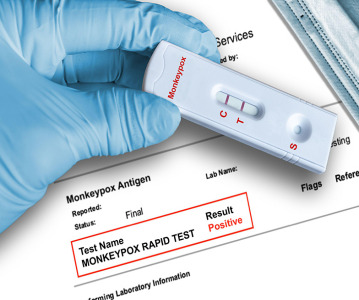
News QIAGEN launches world’s first syndromic test for monkeypox
The test can distinguish between monkeypox and other diseases that cause similar symptoms. -
News Monkeypox Update: Vaccine shortage, sewage surveillance and global testing
As concern over the monkeypox outbreak continues to rise, we take a look at major developments from the first week of August. -
News CPHI Podcast Series: The importance of novel excipients for innovative drug development
The latest episode in the CPHI Podcast Series dives into the world of novel excipients and explores their importance for innovative drug development.
Position your company at the heart of the global Pharma industry with a CPHI Online membership
-
Your products and solutions visible to thousands of visitors within the largest Pharma marketplace
-
Generate high-quality, engaged leads for your business, all year round
-
Promote your business as the industry’s thought-leader by hosting your reports, brochures and videos within your profile
-
Your company’s profile boosted at all participating CPHI events
-
An easy-to-use platform with a detailed dashboard showing your leads and performance


.png)